Full Patient Access and Financial Clearance Outsourcing to Accelerate Revenue.
Outsource Patient Access. Unlock Revenue Growth.
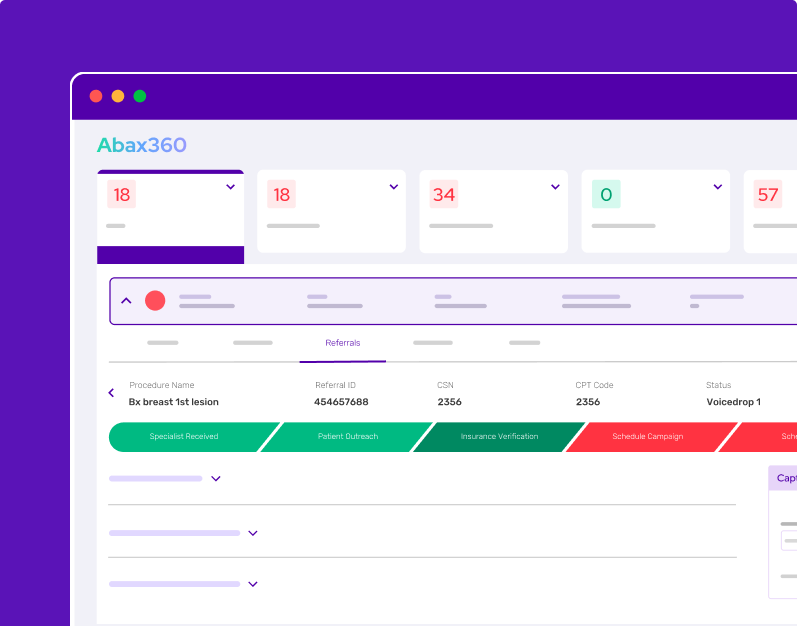
Abax360 is a comprehensive patient access outsourcing solution that helps health systems turn front-end operations into predictable, high-performing revenue drivers. With AI powered and integrated workflow, contact center, and reporting software, expert staff, scalable infrastructure, and industry leading management, we turn your patient access department into a best-in-class operation and flip your patient access department from cost center to a revenue generator.
Because Revenue Starts with Access.
Abax360 is the fastest path to improving your revenue and significantly reducing front end denials. Our model doesn’t just stabilize operations, it actively increases revenue collections by fixing the root causes of your front-end challenges.
Gain immediate access to AI powered workflow, contact center, and reporting software, highly experienced staff, best practice workflows to reduce denials, improve patient satisfaction, and generate new, high margin revenue streams.
Our leadership team brings decades of revenue cycle and patient access experience to maximize your yield from day one. They’ve done this at some of the largest health systems in the country before.
We own the full patient access lifecycle—registration, scheduling, insurance verification, and authorizations, and patient estimations to prevent revenue leakage and improve revenue.
SLAs, dashboards, and cloud-based reporting deliver 360 degrees visibility into your access performance and revenue improvement. Expand services, navigate M&A, or restructure operations without risking performance or revenue for scalable growth.
Faster, more reliable access increases patient retention and revenue.
Identify gaps in your patient access department and revenue losses due to inefficiencies.
Build a revenue centric full outsourcing model tailored to your system’s structure.
Our team executes best-in-class AI powered software and workflows to stop revenue bleed and accelerate collections.
Ongoing analysis helps you scale what works and capture even more revenue.
“Abax360 completely stabilized our patient access departments—and did it faster than we thought possible. We’re seeing a clear improvement in both revenue and patient satisfaction.”
System Director of Revenue Cycle
Abax360 is an enterprise-ready patient access as a service platform that replaces fragmented operations with a centralized, performance-driven model. It is designed to increase collections, reduce denials, and improve patient and staff experience—without adding headcount.
Provides end-to-end best in class management of all patient access, front end, and financial clearance departments.
Delivers intelligent task routing, real-time alerts, and optimized agent performance across the entire patient access lifecycle.
Manages all insurance verification, authorization, and patient estimation services to reduce front end denials.
A team of patient access and revenue cycle leaders oversees execution, performance monitoring, and optimization, bringing decades of health system experience.
Quickly adapts to new sites, departments, or service lines—ensuring continuity during expansions, consolidations, or transitions.
Cloud-based analytics provide real-time visibility into KPIs, staffing efficiency, patient throughput, and revenue performance.
Applies best practices across scheduling and financial clearance to prevent denials before they occur—improving claim accuracy and reducing write-offs.
Ensures fast, reliable access to care with minimized wait times, consistent communication, and fewer breakdowns across scheduling and intake.
Rapid implementation with minimal disruption to internal teams, including assessment, process redesign, and full operational transition.
Transforms patient access into a consistent revenue engine, with documented gains in collection rates, margin, and monthly revenue predictability.
Abax360 offers full-service patient access and financial clearance outsourcing, covering registration, scheduling, insurance verification, authorizations, and patient estimations. It combines AI powered software, expert staffing, and proven workflows to eliminate denials, reduce administrative burden, and generate measurable revenue growth.
Abax360 transforms patient access from a cost center into a revenue driver by addressing the root causes of revenue leakage. Through integrated workflows, real-time reporting, and performance management, it improves scheduling accuracy, reduces delays, and ensures patients move through the front-end process without unnecessary denials or missed opportunities—leading to higher collection rates and predictable monthly revenue.
Yes. Abax360 is built for scalability. Whether you’re expanding locations, integrating after a merger, or restructuring departments, the platform adapts to your volume and complexity. Its modular model allows health systems to maintain access performance and revenue continuity—even during times of rapid change.